Guideline Updates
- Diagnosis, Assessment, and Management of Cough in Children and Adults (CICADA): A Summary of the Updated Position Statement on Chronic Cough in Australia
- Key Clinical Practice Points on Managing Chronic Cough in Adults: Insights from the British Thoracic Society
- International consensus statement on quality standards for managing children/adolescents with bronchiectasis from the ERS CRC Child-BEAR-Net
- WAO-ARIA consensus on chronic cough – Part III: Management strategies in primary and cough-specialty care
- Canadian Thoracic Society 2021 Guideline update: Diagnosis and management of asthma in preschoolers, children and adults
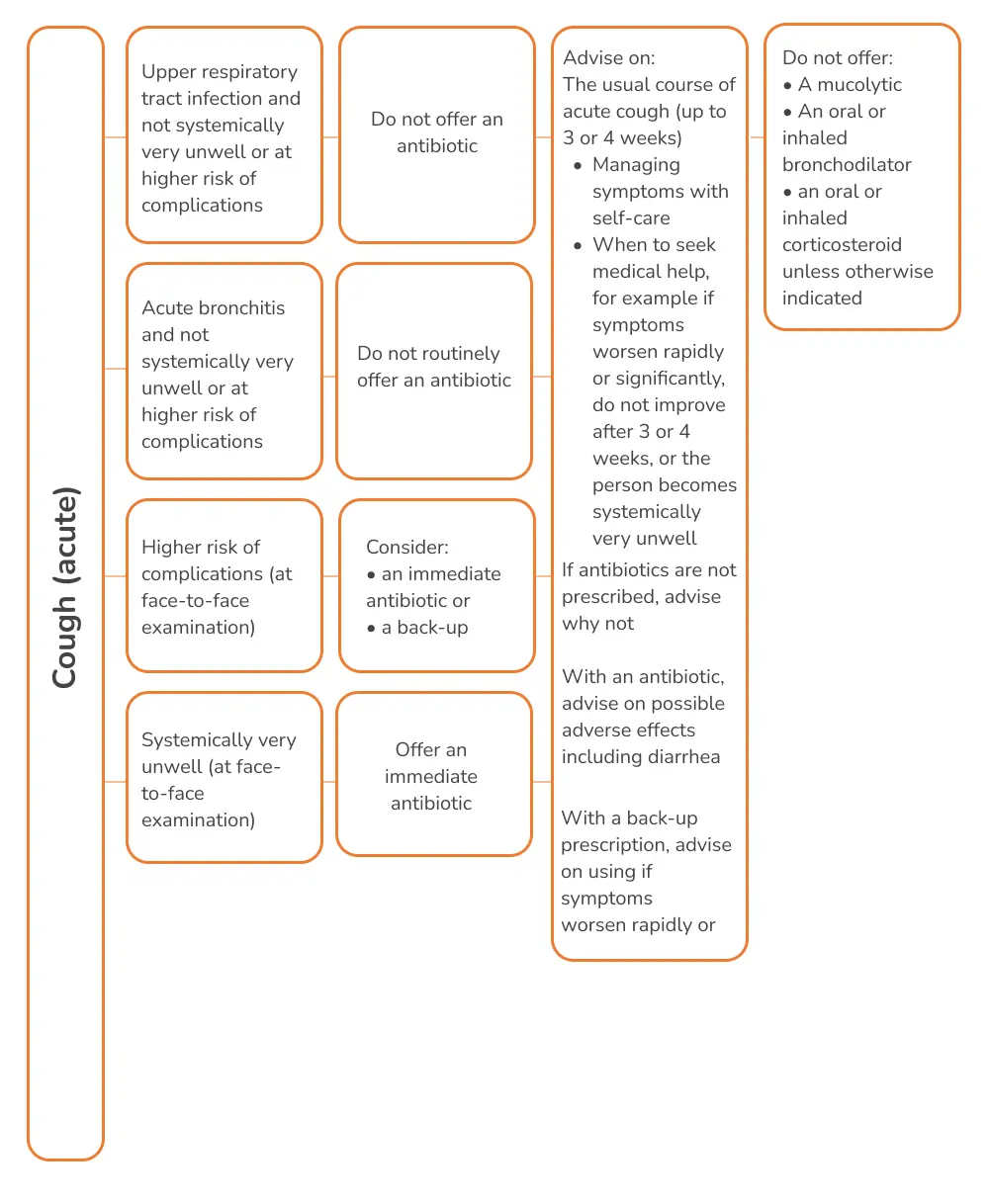
- NICE 2021 guidelines on Cough (acute): Antimicrobial prescribing
- ERS guidelines on the diagnosis and treatment of chronic cough in adults and children
Diagnosis, Assessment, and Management of Cough in Children and Adults (CICADA): A Summary of the Updated Position Statement on Chronic Cough in Australia

A newly updated Australian position statement on the diagnosis and management of chronic cough, Cough in Children and Adults: Diagnosis, Assessment, and Management (CICADA), has been released to standardize clinical approaches and highlight the significant burden of chronic cough, particularly within First Nations communities.
The guidelines offer recommendations for the initial assessment of chronic cough, including identifying key red flags in patient history and examination. Separate diagnostic algorithms have been developed for children and adults, recognizing that the underlying causes of chronic cough differ between the two groups. The guidelines emphasize the need for tailored management strategies based on the latest high-quality evidence.
The updated CICADA statement was developed by a multidisciplinary team of experts who conducted a comprehensive review of recent research. Of the 6,395 articles reviewed, 277 new studies published since 2010 were included in this update. The guidelines use the GRADE system to evaluate the effectiveness of treatment recommendations for chronic cough, ensuring evidence-based care
Overview of Cough as a Clinical Concern
Cough is the most common symptom leading to medical consultations. Chronic cough, in particular, results in significant healthcare costs, impairs quality of life, and may signal the presence of a serious underlying condition. This summary outlines key points from the updated position statement on chronic cough management during clinical consultations.
Main Recommendations
Assessment of Chronic Cough in Children and Adults
- A focused history of chronic cough is essential to identify any red flag symptoms, which may indicate an underlying disease.
- Further assessments should include:
- Chest X-ray
- Spirometry (for patients over 6 years old)
- Separate diagnostic and management algorithms for pediatric and adult chronic cough should be followed.
Management of Underlying Conditions
- Treatment should follow specific disease guidelines for the underlying condition.
- Address adverse environmental exposures that may exacerbate cough.
- Consider patient and caregiver concerns during management.
- First Nations adults and children are classified as a high-risk group and should receive tailored care.
Changes in Management as a Result of the Statement
- Algorithms for assessment and diagnosis of chronic cough are recommended for both adults and children.
- High-quality evidence supports the use of child-specific chronic cough management algorithms, leading to improved clinical outcomes, though such algorithms are currently lacking for adults.
- Red flags signaling serious underlying conditions should be identified early to prompt investigation or referral.
- Early and effective treatment of chronic wet/productive cough in children is critical.
- Culturally specific strategies should be adopted for managing chronic cough in First Nations populations.
- If the chronic cough is unresolved or unexplained, referral to a respiratory specialist or cough clinic is recommended.
To know more: https://doi.org/10.5694/mja2.52157
Reference: Marchant JM, et al. Cough in Children and Adults: Diagnosis, Assessment and Management (CICADA). Summary of an updated position statement on chronic cough in Australia. Medical Journal of Australia. 2024 Jan 15;220(1):35-45.
Key Clinical Practice Points on Managing Chronic Cough in Adults: Insights from the British Thoracic Society

Clinical Practice Points on Chronic Cough Management
Overview:
Chronic cough (CC) predominantly affects middle-aged females and significantly impairs quality of life (QoL). It is associated with increased healthcare costs and often lacks effective management strategies in routine clinical practice.
Diagnosis and Referral
Initial Assessment:
- Obtain a detailed history to identify possible underlying diseases and treatable traits.
- Perform essential tests including a chest X-ray (CXR), full blood count (FBC), diagnostic spirometry, and fractional exhaled nitric oxide (FeNO) if available.
Referral Criteria:
- Refer patients to secondary care if cough persists despite treatment, if the diagnosis remains unclear, or if there is suspicion of underlying conditions such as bronchiectasis, interstitial lung disease, tuberculosis, or heart failure.
- Urgent referral is required for red flag symptoms suggestive of malignancy, following NICE guidelines.
- For predominant upper airway symptoms, consider referring to an ENT service.
Management Strategies
Smoking Cessation
- Encourage smoking cessation as it resolves chronic bronchitis and reduces cough. Nicotine replacement therapy may prevent rebound cough sensitivity.
ACE Inhibitors
- Discontinue ACE inhibitors in all patients with CC. If needed, switch to an angiotensin II receptor blocker (A2RB). Improvement may take up to 4 weeks.
Airway Disease
- For productive cough, investigate possible infections, smoking, or airway diseases such as bronchiectasis. Optimize airway clearance and consider low-dose macrolide therapy, like Azithromycin.
Eosinophilic Airway Disease
- In the absence of airway disease features, avoid inhaled corticosteroids (ICS) and explore alternative causes. In cases with airway disease, manage according to disease-specific guidelines. Consider a 1-month trial of ICS for elevated T2 biomarkers.
Gastro-oesophageal Reflux Disease (GERD)
- Treat with PPIs only if there is clear evidence of acid reflux, such as heartburn. PPIs are not recommended for isolated cough symptoms. Fundoplication is not advised for cough alone.
Upper Airway Symptoms
- For chronic rhinosinusitis (CRS), an empirical trial of a nasal steroid may be beneficial. Avoid using PPIs for throat symptoms.
Obstructive Sleep Apnoea (OSA)
- Consider OSA as a treatable trait in refractory cough. CPAP treatment may improve cough if OSA is confirmed by a sleep study.
Obesity
- Recommend weight loss for obese patients, as it may improve chronic cough.
Cough Hypersensitivity
- Recognize cough hypersensitivity as a treatable trait. It often requires specific treatments, including non-pharmacological approaches, low-dose morphine, or gabapentin.
Specialist Care
- Establish secondary care cough clinics and consider integrating specialist speech and language therapy and physiotherapy into a multidisciplinary team (MDT) for comprehensive management.
Future Directions
- Novel therapies, such as P2X3 antagonists, are under development and show promise for managing chronic cough.
To know more
https://doi.org/10.1136/thorax-2023-220592
International consensus statement on quality standards for managing children/adolescents with bronchiectasis from the ERS CRC Child-BEAR-Net
Eur Respir J. 2022;59(6):2200264
Bronchiectasis is a clinical syndrome encompassing recurrent or persistent wet/productive cough with abnormal bronchial dilatation as seen in chest computed tomography (CT) images.
While the quality of care for people with bronchiectasis is inequitable, the ELF-PAG for the European Respiratory Society (ERS) clinical practice guideline for managing bronchiectasis in children and adolescents expressed the urgent need for standardised quality care.
What exists and what is needed?
- Quality standard statement based on the Birtish Thoracic Society (BTS) guidelines are available for the management of bronchiectasis in adults in the UK and other European countries.
- However, such documents are currently not available for bronchiectasis in children.
- The Child-BEAR-Net (Children’s Bronchiectasis Education, Advocacy and Research Network) aimed to fill this gap.
Quality standard statements for clinically significant bronchiectasis in children and adolescents
The CRC panel and European Lung Foundation-established parent advisory group (ELF-PAG) unanimously and independently endorsed these seven quality standard statements.
References:
Chang AB, Boyd J, Bush A, et al. International consensus statement on quality standards for managing children/adolescents with bronchiectasis from the ERS CRC Child-BEAR-Net. Eur Respir J. 2022;59(6):2200264.
WAO-ARIA consensus on chronic cough – Part III: Management strategies in primary and cough-specialty care
- This third part of the WAO/ARIA consensus on chronic cough suggests a management algorithm of chronic cough in an integrated care pathway approach.
Empirical treatment in primary care
Oral antihistamine therapy in patients with rhinitis and cough is not recommended because of their low efficacy in reducing cough.
Upper airway
- 4-week therapy with intranasal corticosteroids in allergic rhinitis (AR) patients with upper airway disease-related cough.
- Therapy can be tapered in patients showing improvement.
- Patients with partial or no improvement can be referred to cough specialty care.
Lower airway
- No clear role of pharmacotherapy.
- An initial 2-week empirical trial of short-acting bronchodilator supplemented with inhaled corticosteroids (ICS) may be warranted in chronic cough patients.
- If patient cannot tolerate ICS, a short course of oral corticosteroids can be prescribed.
Gastrointestinal (GI) tract
- Behavioral changes (e.g., weight reduction and dietary changes) are recommended in patients with GERD irrespective of concomitant cough.
- An initial 4–12-week empirical and diagnostic trial of proton pump inhibitors (PPIs) can improve a proportion of patients (confirming diagnosis of GERD-related cough).
- PPI therapy can be tapered to the lowest dose for control of cough.
- Patient should be referred to a GI specialist for further investigation of underlying gastrointestinal disorders or in case of PPI failure/dependency.
Guidelines and expert consensus in cough pharmacotherapy
Upper airways
- The role of pharmacotherapy is inconclusive.
Lower airways
- Clinical profile reminiscent of asthma: Several drugs can be offered; studies suggest improvement cough scores with ICS, leukotriene receptor antagonists (LTRAs), inhaled beta2-agonists and muscarinic receptor antagonists, and extent theophylline and mast cell stabilizers (lesser extent).
- Suspected cough-variant asthma (CVA): Recent guidelines recommend ICS as first line treatment. Careful interpretation of the benefit of ICS in nonspecific cough is required.
- Suspected non-asthmatic eosinophilic bronchitis (NAEB): A therapeutic/diagnostic trial of ICS followed by LTRAs (if stepping up ICS fails to improve cough).
- Chronic obstructive pulmonary disease (COPD): An empirical trial of bronchodilator therapy is often justified but requires more efficacy data.
Digestive tract
- Early (within 2 weeks) cough improvement on PPIs, followed by 4–12 weeks of maintenance therapy before tapering medications. Night-time magnesium and melatonin supplementation is recommended for partial responders.
- Supplementing PPI therapy with prokinetics can enhance gut motility and improve gastroesophageal reflux disease (GERD)-related cough.
- Adding H2-blockers for 2–4 weeks can reduce nocturnal acid breakthrough in difficult-to-treat cases of GERD (role in cough has not been investigated).
- Neuromodulators (e.g., baclofen) in combination with PPI can benefit patients with loose lower esophageal sphincter or high reflux symptom index (RSI) scores.
Reference: Rouadi PW, Idriss SA, Bousquet J, et al. WAO-ARIA consensus on chronic cough – Part III: Management strategies in primary and cough-specialty care. Updates inCOVID-19. World Allergy Organ J. 2022;15(5):100649.
Canadian Thoracic Society 2021 Guideline update: Diagnosis and management of asthma in preschoolers, children and adults

An overview of pharmacologic treatment recommendations
- Consider the type of inhaler device that a patient prefers to use and can use properly before prescribing asthma medication
- All asthmatics should have access to a releiver to treat acute symptoms
- In Canada, short-acting beta-agonists (SABAs; salbutamol, terbutaline), and a combination inhaler (bud/form) are approved for this indication.As needed bud/form is approved for use as a reliever in adults and children ≥12 years of age (in Canada).
- Bud/form should not be used as a reliever when controller medications other than maintenance bud/form are used.
- SABAs should only be used for symptom relief and should not be regularly used “to open the airways” before daily controller therapy administration.
- The safest and minimum effective inhaled corticosteroids (ICS) dose that achieves the goals of current control and eliminates exacerbations, should be prescribed to minimize side effects (all groups).
- In poorly controlled asthma cases , potential should be assessed and corrected prior to or in conjunction with escalation of pharmacologic therapy.
Patients not on controller therapy
- Well controlled on SABA or no medication with a lower risk for exacerbations : Continue PRN SABA or be switched to either daily ICS + PRN SABA (all ages) or PRN bud/form (≥12 years of age
- Well-controlled on PRN SABA or no medication with higher risk for exacerbations : Should not be on PRN SABA; switch to daily ICS + PRN SABA (all ages) or PRN bud/form (≥ 12 years of age)
- Not controlled on PRN SABA or no medication : Daily ICS + PRN SABA
- Second line to daily ICS : Leukotriene receptor antagonists (LTRAs) in patients of all ages
Patients not achieving control on low dose ICS
Children not achieving asthma control despite adherence to low dose ICS should be increased to medium dose ICS.
Reference: Yang CL, Hicks EA, Mitchell PA, et al. Canadian Thoracic Society 2021 Guideline update: Diagnosis and management of asthma in preschoolers, children and adults. Canadian J Resp Crit Care Sleep Med. 2021;5(6): 348–361.
NICE 2021 guidelines on Cough (acute): Antimicrobial prescribing
According to the committee discussion, acute cough, either associated with an upper respiratory tract infection or acute bronchitis, is usually a self-limiting infection. It is often a viral infection, and antibiotics are not usually needed.
Recommendations on when antibiotics are not required, are required immediately, or as back-up
Recommendations on the choice of antibiotic
- A narrow-spectrum antibiotic should generally be first choice, when an antibiotic is needed.
- Where an antibiotic is appropriate, doxycycline at usual dose is recommended, as the first-choice antibiotic for adults with acute cough (including acute bronchitis), in non-pregnant adults, and in young people >12 years.
- Amoxicillin, clarithromycin or erythromycin should be offered as alternative first choices; for children and young people, amoxicillin is recommended as the first-choice antibiotic in such scenario.
Recommendations on antibiotic course length
- The shortest course that is likely to be effective should be prescribed. A 5-day course for all the recommended antibiotics is sufficient to treat acute cough.
Reference: NICE guideline. Available at www.nice.org.uk/guidance/ng120
ERS guidelines on the diagnosis and treatment of chronic cough in adults and children
According to the guideline panel, it is preferable to undertake sequential therapeutic trials of each agent in turn and if no responses are observed therapy should be stopped. The length of the trial depends on the pharmacology.
Pharmacological control
Recommendations for using anti-asthmatics
- A short-term ICS trial (2–4 weeks) in adult patients with chronic cough
- A short-term ICS trial in children with chronic dry cough (2–4 weeks)
- A short-term antileukotriene trial (2–4 weeks) in adults with chronic cough, particularly in those with asthmatic cough
- A short-term trial (2–4 weeks) of ICS and long-acting bronchodilator combination in adults with chronic cough and fixed airflow obstruction
Recommendations for using anti-acids
- It is recommended that clinicians do not routinely use anti-acid drugs in adult patients with chronic cough
Recommendations for using drugs with promotility activity
- There is currently insufficient evidence to recommend the routine use of macrolide therapy in chronic cough. A 1-month trial of macrolides can be considered in the cough of chronic bronchitis refractory to other therapy, considering local guidelines on antimicrobial stewardship.
Recommendations for using neuromodulatory agents
- A trial of low-dose morphine (5–10 mg twice daily) in adult patients with chronic refractory cough we suggest a trial of gabapentin or pregabalin in adult patients with chronic refractory cough.
Nonpharmacological control
- A trial of cough control therapy in adult patients with chronic cough is recommended.
Antibiotics for chronic wet cough in children
- A trial of antibiotics is suggested in children with chronic wet cough with normal chest radiographs, normal spirometry and no warning signs.
Reference: Morice AH, Millqvist E, Bieksiene K, et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J. 2020;55(1):1901136.

An initiative by Glenmark to educate about everything related to Cough and spread awareness about cough related health conditions.
Quick Links
Contacts
- GLENMARK PHARMACEUTICALS LIMITED Glenmark Corporate Enclave, BD Sawant Marg, Chakala, Off WE Highway, Andheri (E), Mumbai 400099
- Terms & Condition
- Privacy Policy
- Sitemap
- Disclaimer
- Coughology © 2024 All Right Reserved
